Get enterprise-wide results with Hyland Healthcare
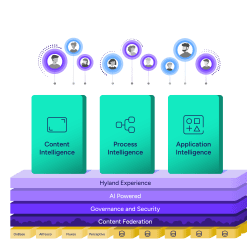
Is there a disconnect between the goals of your healthcare organization and the organization’s current reality? We can help. Explore how our intelligent content and enterprise imaging solutions improve information access, connect systems and processes, and enhance patient experiences.