Future-proofing the healthcare payer infrastructure
There is a new paradigm for healthcare payer organizations. Prepare for the future with the technology you need to seize new opportunities.
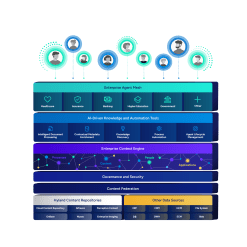
Harness the power of a unified content, process and application intelligence platform to unlock the value of enterprise content.
Learn more
Automate your document-centric processes with AI-powered document capture, separation, classification, extraction and enrichment.
Learn about Hyland IDPIt's your unique digital evolution … but you don't have to face it alone. We understand the landscape of your industry and the unique needs of the people you serve.
 Overview of industries
Overview of industries
Countless teams and departments have transformed the way they work in accounting, HR, legal and more with Hyland solutions.
 Overview of departments
Overview of departments
We are committed to helping you maximize your technology investment so you can best serve your customers.
 Overview of services
Overview of services

You’re shaping the future, now it’s time to celebrate your achievements at CommunityLIVE 2026.
Submit your Hyland Innovation Award nomination!
Our exclusive partner programs combine our strengths with yours to create better experiences through content services.
Overview of partners
Join The Shift newsletter for the latest strategies and expert tips from industry leaders. Discover actionable steps to stay innovative.
Register now
Hyland connects your content and systems so you can forge stronger connections with the people who matter most.
Learn about HylandWith our modern, open and cloud-native platforms, you can build strong connections and keep evolving.
 Dig deeper
Dig deeper
After payers helped their employees make the abrupt shift to work-from-home, and after the dust settled, many found themselves contemplating a comprehensive review of their technology infrastructure. Small cracks in the road to digital transformation had widened and could no longer be ignored.
But COVID-19 was hardly a lone disruptor for payers. Pressures were building for some time from new competitors, regulatory agencies, providers, partners and the new digital-first consumer.
So, now what? What changes are needed to pave a smoother, more resilient highway to the future?
— Prepare for the Next Business Stress-Test with Content Services, Forrester Consulting, March 2021
Payers finding their way in this new era are looking for technology infrastructure changes that can best strengthen their resilience, performance and agility. I see three challenges that commonly surface in payer organizations I’ve talked with where there is great opportunity for change and ROI. They are:
Technology infrastructure changes that address business goals are paramount. Over the years, we’ve seen the incredible positive impact that content-centric strategies can have on payer organizations in addressing challenges and meeting business goals. Today, they’re accelerating adoption of cloud, intelligent capture, and process automation and looking for low- and no-code solutions to help achieve operational excellence.
Here are a few examples of what payers are doing to transform their content management strategy:
Again, the right cloud-based content services platform with intelligent automation can change the game for the healthcare payer. Our customers have pointed to reductions of more than 50 percent in quarterly reporting, 95 percent improvement in appeals and grievances processes and achievement of 98 percent accuracy and timeline goals. This payer, recipient of a four-star rating for its Medicare plans in 2020 and 2021, entirely transformed its appeals and grievances process with Hyland.
There is a new paradigm for payer organizations. Is your organization prepared with the technology it needs to be nimble, adaptable to change? Ready to pivot and seize new opportunities? If you’d like to know more, I’m happy to chat!
Learn more about Hyland solutions for healthcare payers.